Blog
7 mistakes to avoid when implementing secure messaging
Secure messaging solutions, designed specifically for healthcare as a HIPAA-compliant method of communication that protects patient privacy, have been around since the mid-to-late 2010s and continue to grow in popularity.
In fact, in our latest iteration of the State of Healthcare Communication Report, 93% of participants named “secure messaging” as a preferred feature for their clinical communication and collaboration (CC&C) platforms for the second year in a row. Furthermore, 85% described “secure messaging” as part of their current technology usage, speaking to the importance of meeting compliance requirements.
If your hospital is ready to implement a secure messaging service among your employees, it’s worth considering the potential challenges that come with adopting any new platform or tool. For maximum success, avoid these seven potential mistakes.
1. Creating a project team with the wrong stakeholders
Deploying a secure messaging solution is an enterprise project that affects clinical departments, contact centers, and hospital administrations. Many healthcare organizations undergo this process with a project team that consists only of clinicians and IT personnel.
From project kickoff to ongoing optimization, it’s critical to have a diverse group of stakeholders involved and committed to the project. Additional employees from clinical informatics, contact center operations, and executive administration can offer essential insights about secure messaging software based on their unique roles and responsibilities.
2. Having poor wireless infrastructure
It almost goes without saying, but a reliable wireless infrastructure is essential for implementing a secure messaging platform. An inadequate wireless network can cause message delays or failures, preventing users from trusting their communication applications.
Many hospitals often stall their secure messaging projects due to the shortcomings of their wireless networks, most often seen in rural areas that lack sufficient broadband access.
With a wireless infrastructure audit, your healthcare organization can reveal heat maps of your facilities and determine dead zones where additional access points are needed. Improving your coverage may include extending distributed antenna systems (DAS), upgrading routers, and adding wireless APs.
3. Overlooking success measurements
“You can’t manage what you can’t measure” is a cliché that rings true when deploying secure messaging solutions. Healthcare IT projects often start without documenting precise, objective success measurements.
A hospital’s business drivers should go beyond “improve care team communication” or “safeguard PHI in messages.” For example, UPMC wanted to create a quieter hospital by reducing noise disrupting patient recovery. To achieve this goal, they limited hallway conversations and eliminated overhead paging by converting announcements and discussions into messages.
Measuring secure messaging success looks different for every healthcare organization, but it may include using technology or information gathered from devices, data from HCAHPS scores, direct feedback from end users, and surveys.
4. Failing to integrate your directory
To facilitate faster communication between your care teams, your secure messaging platform should be integrated with a single source of truth for contact details, schedules, and preferences. Users can log onto the application to search the directory, identify who is on call, and send important messages.
Unlike EHRs (electronic health records), which typically only allow access to employees with clinical credentials, an enterprise directory includes all members of care teams—from physicians to nurses to contact center operators to housekeeping staff.
Without an enterprise directory that’s readily accessible and relays real-time updates, your employees will waste their valuable time sorting through outdated information. This can mean a matter of life and death during critical scenarios.
5. Not sending alerts from systems
A secure messaging solution is more than a simple text conversation between two people. Originally known as secure text messaging, this technology has evolved to include middleware integration that sends alarms and alerts from EHR, nurse call systems, and patient care monitoring.
If your hospital can’t connect systems to people, your employees can’t benefit from seamless and efficient workflows. Clinical alerting technology sends critical information and updates from your alert systems to your staff’s mobile devices, creating an enterprise-wide approach to management, prioritization, and response to time-sensitive events.
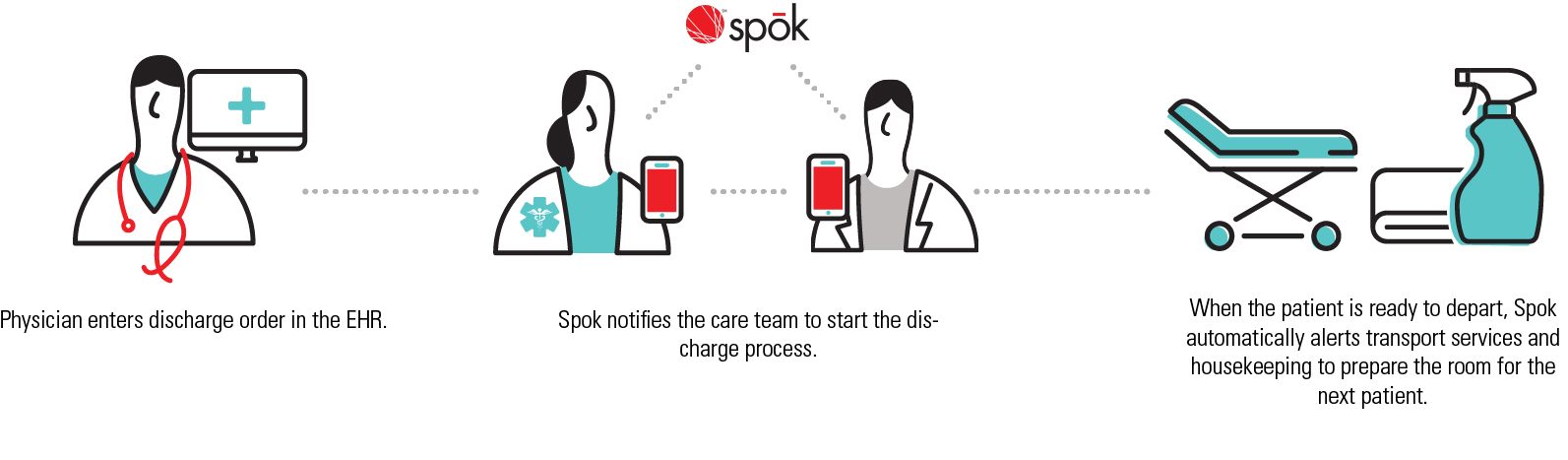
As seen below, secure messaging can eliminate communication gaps during the patient discharge process and ensure that a hospital’s bed occupancy rate remains at an ideal level.
6. Neglecting to educate your end users about the technology
When it comes to clinical communication, technology is just one piece of the puzzle. The entire process—and the people using it—are just as necessary.
Whether you’re presenting a secure messaging solution to a pilot department or rolling it out across your entire healthcare organization, providing education and training is essential.
Be sure to clearly outline the benefits for all end users. Messaging on-call staff is more advantageous to clinicians than other employees at your hospital or health system. Nurses might find more value in receiving alerts from nurse call systems and patient care devices, limiting unnecessary trips to patient rooms and reducing overall alarm fatigue.
Your hospital should invest resources in organizational change management as part of education and training for a new secure messaging service. Our Adoption Services include using the Prosci ADKAR® model to measure the progress of their process.
Education and training about secure messaging shouldn’t end with implementation. It should be treated as an ongoing event as new features are rolled out and new employees join your healthcare organization.
7. Lacking a plan to sustain and optimize the solution
EHRs prove there is no such thing as an “install it and leave it” approach to healthcare technology that’s embedded in clinical workflows. The same goes for secure messaging solutions, where initial implementation is just phase one.
Look beyond the rollout to ensure that you have a plan to reinforce the value of your secure messaging software. For example, your hospital can maintain interest in this powerful communication tool by posting reminders of its benefits in cafeterias and breakrooms or hosting periodic help desk sessions to answer questions.
By outlining these seven common mistakes that hospitals make when rolling out a secure messaging platform, your healthcare organization can confidently avoid them and successfully navigate your way toward clinical collaboration success.
Topic: Secure Messaging







